Gestational Trophoblastic Tumor
Gestational trophoblastic disease (GTD) can be benign or malignant. Histologically, it is classified into hydatidiform mole, invasive mole (chorioadenoma destruens), choriocarcinoma, and placental site trophoblastic tumor (PSTT). Those that invade locally or metastasize are collectively known as gestational trophoblastic neoplasia (GTN). Hydatidiform mole is the most common form of GTN. While invasive mole and choriocarcinoma are malignant, a hydatidiform mole can behave in a malignant or benign fashion .Histologic section of a complete hydatidiform mol...Histologic section of a complete hydatidiform mole stained with hematoxylin and eosin. Villi of different sizes are present. The large villous in the center exhibits marked edema with a fluid-filled central cavity known as cisterna. Marked proliferation of the trophoblasts is observed. The syncytiotrophoblasts stain purple, while the cytotrophoblasts have a clear cytoplasm and bizarre nuclei. No fetal blood vessels are in the mesenchyme of the villi.
 No methods exist to accurately predict the clinical behavior of a hydatidiform mole by histopathology. The clinical course is defined by the patient's serum human chorionic gonadotropin (hCG) curve after evacuation of the mole. In 80% of patients with a benign hydatidiform mole, serum hCG levels steadily drop to normal within 8-12 weeks after evacuation of the molar pregnancy. In the other 20% of patients with a malignant hydatidiform mole, serum hCG levels either rise or plateau.1,2
No methods exist to accurately predict the clinical behavior of a hydatidiform mole by histopathology. The clinical course is defined by the patient's serum human chorionic gonadotropin (hCG) curve after evacuation of the mole. In 80% of patients with a benign hydatidiform mole, serum hCG levels steadily drop to normal within 8-12 weeks after evacuation of the molar pregnancy. In the other 20% of patients with a malignant hydatidiform mole, serum hCG levels either rise or plateau.1,2
Pathophysiology
A hydatidiform mole is considered malignant when the serum hCG levels plateau or rise during the follow-up period and an intervening pregnancy is excluded. This occurs in 15-20% of hydatidiform moles.1,2,3
A hydatidiform mole with a fetus or fetal tissue and a triploid karyotype is known as a partial or incomplete mole. Partial moles also have malignant potential, but only 2-3% become malignant.4,5,6 Cases of partial hydatidiform moles with lung metastasis have been reported and at least one case of choriocarcinoma on a biopsy from a vaginal metastasis has been reported in a patient being observed for a partial hydatidiform mole.7,8
An invasive mole has the same histopathologic characteristics of a hydatidiform mole, but invasion of the myometrium with necrosis and hemorrhage occurs or pulmonary metastases are present.
Histologically, choriocarcinomas have no villi, but they have sheets of trophoblasts and hemorrhage. Choriocarcinomas are aneuploid and can be heterozygous depending on the type of pregnancy from which the choriocarcinoma arose. If a hydatidiform mole preceded the choriocarcinoma, the chromosomes are of paternal origin. Maternal and paternal chromosomes are present if a term pregnancy precedes the choriocarcinoma. Of choriocarcinomas, 50% are preceded by a hydatidiform mole, 25% by an abortion, 3% by ectopic pregnancy, and the other 22% by a full-term pregnancy.1 Choriocarcinoma has also been associated with ectopic pregnancy with a theoretic incidence of 1 in 5333 ectopic pregnancies.9
Placental site trophoblastic tumor is a rare form of gestational trophoblastic neoplasia, with slightly more than 200 cases reported in the literature.10,11 In patients with PSTT, intermediate trophoblasts are found infiltrating the myometrium without causing tissue destruction. The intermediate trophoblasts contain human placental lactogen (hPL).12 These patients have persistent low levels of serum hCG (100-1000 mIU/mL). However, serum hCG levels as high as 108,000 mIU/mL have been reported in patients with PSTT.13 The treatment of PSTT is hysterectomy with ovarian conservation.14 If the tumor recurs or metastases are present at initial diagnosis, chemotherapy is administered with variable results.15,16 Radiation therapy may provide local control.
The most frequent sites of metastases of malignant gestational trophoblastic neoplasia are the lungs, lower genital tract, brain, liver, kidney, and gastrointestinal tract.
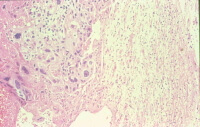 In this microphotograph of a choriocarcinoma metastatic to the brain, the neuropil is seen on the right and the biphasic (2 cell populations) choriocarcinoma is seen to the left with hemorrhage at the left border of the photograph (H&E stain).
In this microphotograph of a choriocarcinoma metastatic to the brain, the neuropil is seen on the right and the biphasic (2 cell populations) choriocarcinoma is seen to the left with hemorrhage at the left border of the photograph (H&E stain).
Frequency United States
Gestational trophoblastic neoplasia is diagnosed in 15-20% of patients with a complete hydatidiform mole and 2% of partial hydatidiform moles. Lung metastases are found in 4-5% of patients with complete hydatidiform moles and rarely in cases of partial hydatidiform moles.
Choriocarcinoma occurs in 1 out of 40 hydatidiform moles and in 1 out of 20,000-40,000 pregnancies.However, only 1 out of 160,000 term pregnancies is followed by a choriocarcinoma.
International
The international rate of choriocarcinoma has been reported to be as high as 1 in 500-600 pregnancies in India to 1 in 50,000 pregnancies in Mexico, Paraguay, and Sweden.,These differences are probably due to differences in methodology (eg, identification of cases, accuracy of denominator)
Mortality/Morbidity
Patients who have a malignant hydatidiform mole, an invasive mole, or a choriocarcinoma should undergo a systematic search for metastases. Patients who have metastases are classified as high-risk or low-risk according to the National Institutes of Health classification.The criteria for high-risk metastatic gestational trophoblastic neoplasia include hepatic or brain metastasis, serum hCG levels greater than 40,000 mIU/mL prior to the initiation of chemotherapy, duration of disease longer than 4 months, prior unsuccessful chemotherapy, and malignant gestational trophoblastic neoplasia following a term pregnancy.
- Patients with malignant nonmetastatic or metastatic low-risk gestational trophoblastic neoplasia have an almost 100% probability of cure with chemotherapy. The probability of cure after chemotherapy for patients with metastatic high-risk gestational trophoblastic neoplasia is approximately 75%.
- The probability of a late recurrence after the patient has been in remission (normal serum beta-hCG titers) for 1 year is less than 1%.
Race
- Little information is available on international ethnic or racial differences of the incidence of choriocarcinoma. In Singapore, Malaysians have the highest incidence.
- In the United States, African Americans have the highest incidence of choriocarcinoma and the lowest survival rates.
Sex
Gestational trophoblastic neoplasia affects women during their reproductive years. However, placental site trophoblastic tumors have been diagnosed when patients were postmenopausal.
Age
The incidence of choriocarcinoma increases with age and is 5-15 times higher in women 40 years and older than in younger women.19
Clinical History
Most cases of gestational trophoblastic neoplasia are diagnosed when the serum hCG levels plateau or rise in patients being observed after the diagnosis of hydatidiform mole. If metastases are present, signs and symptoms associated with the metastatic disease, such as hemoptysis, abdominal pain, hematuria, and neurologic symptoms, may be present.
Physical
- Metastasis to the lower genital tract present as purple to blue-black papules or nodules. These are extremely vascular and might bleed profusely if biopsied.
- Abdominal tenderness may be present if liver or gastrointestinal metastases have occurred.
- Abdominal guarding and rebound tenderness may be present if a hemoperitoneum has occurred due to bleeding from an abdominal metastasis. Bleeding from a metastasis could also result in signs and symptoms of hemorrhagic shock.
- Neurologic deficits, from lethargy to coma, can be encountered if brain metastasis has occurred.
- Jaundice may be present if liver metastasis causes biliary obstruction.
Causes
Why some hydatidiform moles become malignant and others do not is unknown. However, mounting evidence shows different molecular profiles between nonmalignant and malignant gestational trophoblastic disease